Fix your ED capacity and wait times
Also: review the Envision story, Indiana signs new law, new NP/PA pay data, Amazon is everywhere, and NPs & PAs making a difference
Top of the week
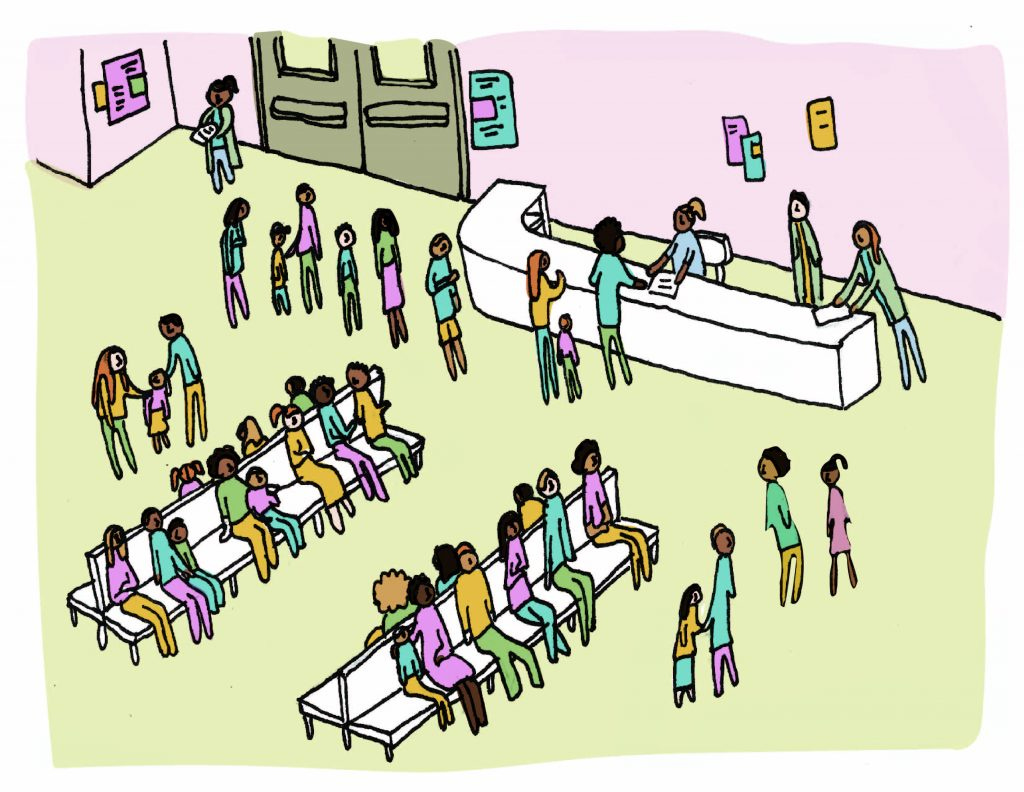
What is the solution for dilution for ED waiting rooms?
It is no secret that everybody reading this has experienced firsthand, or at least second hand, the patient capacity problems in the ED. Certainly, the Covid pandemic maximized capacity problems. Average ED wait times by state were reviewed over a period of January 2020 and March 2021. Check out where your state ranks. However, have capacity problems and ED wait times improved so much in the post covid era? In 2022 we saw the triple threat of RSV, flu, and Covid remnants. Places like Kansas City and Michigan were overrun. It has become common place, for the past 1- 2 years, to arrive on shift with all ED beds filled with admission/transfer holds. EDs share a number of similar challenges, but there are differences also. This article cites four interventions to address ED capacity challenges. Some of you may have tried some of these interventions in your department. Perhaps you’ve tried all of them. Not every intervention is a solution for every ED. In the end, you can only replace missing nursing hours with nursing hours, not with more work out of the providers.
Emergency Medicine
Quick review of what happened to Envision
I know I covered this before, but I wanted to share this succinct review of what happened to Envision. This is not an attempt to “pile on.” I once worked for EmCare, myself. I do think it’s important to identify factors that contributed to the bankruptcy of a major staffing company acquired by a private equity firm. It is very likely that some of those factors are common to other major private equity backed staffing companies. One such common challenge was the end of balance billing. With less money coming for staffing companies, I suspect a corridor is opening for new, smaller physician-owned groups to grab a share of the ED market.
The doctor is always in
Having a physician on site in the ED absolutely sounds completely logical and responsible. Who could oppose wanting a physician on site in any ED? I do think, however, it would be useful to identify any U.S. remote EDs that currently do not have physicians on site because they have never been able to recruit physicians there. This does exist. How many impacted patients are we talking about? Will this action increase patient access to emergency physician care or decrease access to any emergency provider care at all? I believe this deserves close scrutiny and robust debate.
Como se dice “sick patient?”
A recently published study examined the under triaging of ED pediatric patients when the patient’s caregiver was non-English speaking. As our patient population demographics continue to evolve there will be a continued demand for departments to supply a reliable translation resource for ED staff.
House of Medicine
How much should you be paid?
It’s challenging to get a good handle on pay data that is specific and truly meaningful to you when you are trying to negotiate a new job or negotiate a raise at your current job. The Medical Group Management Association (MGMA) recently published APP workforce data. We know that pay varies by states. Check out this best vs worst state list.
NPs & PAs have been fortunate to experience pay raises overall, but how did you fare between 2018 and 2022?
NP & PA bonuses is a separate issue. Check out how many APPs received bonuses, and how much they received.
“Free and Independent States have full Power to establish Commerce”
There is no question that a debate over NP/ PA scope of practice and autonomy has firmly taken hold in this country. Though there may be intentions and efforts by some to address this through national restrictions, I believe that this debate, like many hot topics, will be decided by individual states. Just Look at the recent developments in Utah NP & PA practice. Individual states will have to examine historical trends and future projections of patient access to care vs. available, qualified providers. States will have to decide what’s best for their residents. Check out Iowa’s recent decision.
Hospitals, health systems, and more
Hospitals are trying everything to fill the gaps
Expected shortages among physicians and nurses for the next 10.5 yrs. is shocking. Multiple factors, including Covid, of course, have reshaped the workforce. In turn multiple interventions will be required to repair the shortage. Some folks are looking for better compensation for the demands of working in healthcare. Others are just looking for a lifestyle that doesn’t grind them down. Working in EM is not for everybody. For those that do venture in it, gone may be the era that one worked for 15, 20, 25 years in this specialty.
How far can Alexa go?
Quick read on the growth of one of Amazon’s medical holdings. In February of this year, Amazon paid $3.9 billion for One Medical, a virtual and in-person primary care company. One Medical offers subscriber plans for an annual membership fee. This transaction happened after Amazon decided to end Amazon Care, its telemedicine & in-person healthcare service. In my neck of the woods, there is no shortage of patients saying they have to wait for months to get a PCP appointment. Many of them show up to the ED. Whether we “fast- track” them in the ED triage or make them wait in the waiting room, they impact the ED. The success or failure of Amazon’s newest venture will be interesting to witness over the next 5-10 years.
The Good Stuff
Read about this NP leader who talks about a very familiar theme: NPs & PAs improving patient access to care. Thank you, Cindi. This undeniable reality will require persistent discussion over the next 5-10 years at least.
A Massachusetts PA sets the bar high. Aubrey Stimola Ryan is an inspiring EM PA who also contributes her time and talents abroad.
To NPs & PAs everywhere:
I believe NPs & PAs are working side by side in harmony with physicians in EDs all over America. Access to EM care is being improved, and good quality outcomes are being produced. Many of you are working in remote locations that cannot recruit EPs. There are always opportunities for improvement, but those opportunities should be identified on an individual basis rather than a one-size fits all fashion.
Thank you for all you endure and all you do in order for more patients to have access to quality EM care.
Thanks for reading Emergency NP & PA Workforce Newsletter! Subscribe for free to receive new posts and support my work.
Please check out the new EM NP & PA Workforce podcast and listen to what your colleagues are talking about!
This newsletter is sponsored by Ivy Clinicians, the simplest way for emergency physicians, physician assistants, and nurse practitioners to find jobs they love.